After the initial shock of my gestational diabetes diagnosis, I got down to business. Four times a day, I tested droplets of blood for glucose. I wrote down my scores and meals in a notebook. A friend sent me simple food guidelines. The Gestational Diabetes UK website has been a phenomenal resource. I also attended a brilliant education session at St Thomas’s hospital.
All of the above brought me peace of mind because I discovered:
- there are simple changes I can make in pregnancy, which will help my baby
- gestational diabetes is not my fault – it can be genetic (and there is diabetes in my family)
- it is quite common, especially in the third trimester – around 1 in 20 pregnant women develop gestational diabetes
I began to see this as a great opportunity to soak up advice on nutrition, as although the condition should go away after pregnancy, there is a higher chance of me developing diabetes in later life.
Soon, I learned what food worked for me. I am one of the lucky ones with the choice to manage gestational diabetes with food alone. It felt like a huge reprieve to see my early blood glucose scores come up good – not that there is anything wrong with medication, but being an IVF mum, I have an aversion to yet more medical intervention, unless absolutely necessary.
Another huge positive after the diagnosis has been the surge of motivation to stay active and relaxed. I’ve done a pregnancy yoga video most mornings since week 33 of pregnancy and I’ve upped my walks. I’ve been loving the sunshine and I have meditated everyday to stay chilled, as stress can spike blood sugar.
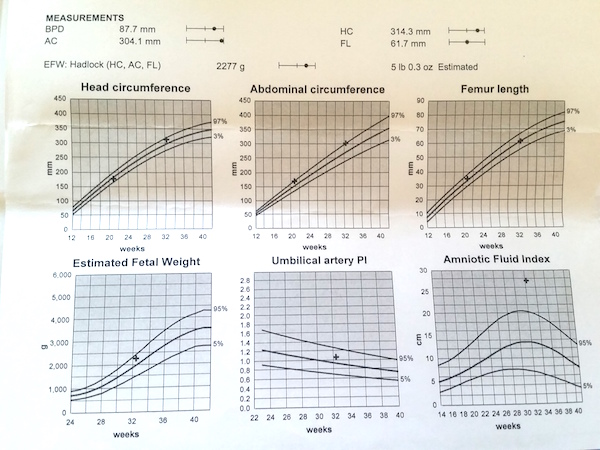
The best news of all is this: at our 34 week and 36 week scans, we saw the impact of the changes I made on our baby. After two weeks, my amniotic fluid came back down within normal levels. After four weeks, our baby’s abdominal measurement had reduced from the 97th centile to the 73rd centile. That was the truly the best feeling – to see the difference it made to our baby.
So, I’m sharing here the main discoveries that have helped me to manage gestational diabetes with a food plan alone. (Please note: these suggestions won’t work for everyone – but hopefully they are a starting point after a gestational diabetes diagnosis).
1) Dairy milk is more carbohydrate than protein
 Before my diagnosis, I didn’t know this! Whilst I knew there was carbohydrate in dairy milk, in the form of lactose, I always thought the white stuff was much higher in protein. There was an old association in my head with body builders, downing pints of milk to bulk up their muscles. Yes, there is protein in dairy milk, but there is actually more carbohydrate.
Before my diagnosis, I didn’t know this! Whilst I knew there was carbohydrate in dairy milk, in the form of lactose, I always thought the white stuff was much higher in protein. There was an old association in my head with body builders, downing pints of milk to bulk up their muscles. Yes, there is protein in dairy milk, but there is actually more carbohydrate.
For me, I found there was no need to restrict dairy milk entirely. I still have ordinary milk in tea, for example, and I used ordinary milk to make a cheese sauce. I just don’t have glasses of the stuff anymore and I switched to an alternative milk at breakfast.
2) Sometimes ‘healthy’ isn’t what it seems
 Initially, I switched to a ‘healthy’ milk alternative to make my porridge. I picked Rude Health unsweetened almond milk because it sounded just the job. Everything about the packaging shouted this was a much better choice for me than semi-skimmed dairy milk. So, I bought it!
Initially, I switched to a ‘healthy’ milk alternative to make my porridge. I picked Rude Health unsweetened almond milk because it sounded just the job. Everything about the packaging shouted this was a much better choice for me than semi-skimmed dairy milk. So, I bought it!
I learned through this experience to read the nutritional labels. Having Rude Health almond milk with porridge spiked my blood glucose to 8.2 (over the 7.0 limit). Thanks to helpful GD mums online, I then switched to Alpro unsweetened almond milk with porridge, which keeps my post-breakfast blood test under 7.0.
3) No more Daddy bear bowls!
 On the subject of porridge, some women with gestational diabetes can tolerate porridge and others can’t. I fall somewhere in the middle. For me, it’s completely down to portion control. One of the main things that I think was spiking me over the blood glucose limit before the diagnosis were the Daddy bear bowls of porridge I gobbled down, two to three times a week. My typical portion before the diagnosis was enough for two adults, according to the recommended serving size. Add to that the lactose in dairy milk, the concentrated sugars in sultanas or dried goji berries, then a chopped apple or banana on top – and really this staple breakfast choice was carbs on carbs on carbs on carbs!
On the subject of porridge, some women with gestational diabetes can tolerate porridge and others can’t. I fall somewhere in the middle. For me, it’s completely down to portion control. One of the main things that I think was spiking me over the blood glucose limit before the diagnosis were the Daddy bear bowls of porridge I gobbled down, two to three times a week. My typical portion before the diagnosis was enough for two adults, according to the recommended serving size. Add to that the lactose in dairy milk, the concentrated sugars in sultanas or dried goji berries, then a chopped apple or banana on top – and really this staple breakfast choice was carbs on carbs on carbs on carbs!
Through weighing out my porridge oats, I discovered that I can tolerate a smaller (aka normal size!) portion of porridge (35-40g), made with Alpro unsweetened almond milk (no carbs), mixed nuts and a handful of berries. I always stir in a spoon of peanut butter too (heaven!).
4) Peanut butter is my lover!
 I’m now obsessed with peanut butter! Fuck, it has literally saved me these last 7 weeks – it’s a total love thing!
I’m now obsessed with peanut butter! Fuck, it has literally saved me these last 7 weeks – it’s a total love thing!
My peanut butter of choice is Pip & Nut, as it is just made with peanuts and salt, no added sugar. I need some food in my life that feels naughty and peanut butter totally does it for me. Okay, so ladelling it down is probably not a great idea, as it’s high fat, but a spoonful of Pip & Nut transforms me from feeling deprived to feeling totally satisfied!
5) Breakfast is now way more interesting
 Having gestational diabetes challenged me to vary my breakfasts. For a long time, we did a three-day rotation in our household between the following:
Having gestational diabetes challenged me to vary my breakfasts. For a long time, we did a three-day rotation in our household between the following:
- Daddy bear bowl of porridge with fruit
- Eggs of all kinds on toast
- Some combination of avocado, tomatoes and mushroom on toast
After the GD diagnosis, I started to think about a protein base for all my breakfasts. I still need some carbs in my breakfast, as without that balance I’m starving by 10.30.
These are some of the breakfasts I’ve really enjoyed and they have kept my post-breakfast blood glucose reading under 7.0:
- Smoked salmon and cottage cheese on granary or sourdough toast (1-2 slices are okay for me, but this varies person to person)
- Grilled mackerel with asparagus and lemon, on granary or sourdough toast spread with Philadelphia cheese
- Homemade houmous with vegetable crudités and hardboiled eggs
- Mozzarella (either hard or soft) with grilled cherry tomatoes and basil on granary or sourdough toast
- Peanut butter porridge (max 35-40g) with Alpro unsweetened almond milk, soaked mixed nuts and berries
- Eggs of any kind with spinach, followed by mixed berries and natural yoghurt
- Scrambled tofu, garlic mushrooms, spinach and tomatoes (I had this out at a vegetarian breakfast café and it was deeee-licious!)
- Avocado with lime, chilli & mixed seeds with boiled egg and toast
6) How to plate up lunch
 Mainly, I’ve eaten my biggest meal of the day at lunch. This was suggested by our hospital, as I am more likely to burn off excess carbohydrates with activity during the day.
Mainly, I’ve eaten my biggest meal of the day at lunch. This was suggested by our hospital, as I am more likely to burn off excess carbohydrates with activity during the day.
The diabetes nurse suggested dividing up the plate this way:
- a quarter of the plate protein
- a quarter carbohydrate
- half the plate of non-starchy vegetables (ideally a variety including greens)
7) Berry heaven and the useful fruit rule!
 Berries have become my sweetest friend. I learned at the St Thomas’s hospital education session a rule of thumb about fruit sugar. Generally speaking, the closer a fruit grows to the equator, the higher the sugar content. So northern hemisphere fruits, as a general rule, are lower in sugar.
Berries have become my sweetest friend. I learned at the St Thomas’s hospital education session a rule of thumb about fruit sugar. Generally speaking, the closer a fruit grows to the equator, the higher the sugar content. So northern hemisphere fruits, as a general rule, are lower in sugar.
Strawberries, raspberries, blueberries work well for me. Pears are better for my blood glucose score than apples. I steer clear of bananas, pineapple, mangoes, figs, all dried fruit and fruit juices, as well as big bowls of fruit salad. Here’s a helpful list of glycemic load in fruits.
I have come to really love a small bowl of mixed berries with natural yogurt and some mixed nuts – it might sound boring but eating a ripe strawberry, very slowly, is a sensational experience!
8) Eggs – my most faithful friend!
 When my post-breakfast scores veered too close to the 7.0 mark, I reverted to eggs.
When my post-breakfast scores veered too close to the 7.0 mark, I reverted to eggs.
Eggs have never failed me, including served on toast.
Good quality protein and fat, B vitamins, vitamin D, selenium and more goodness besides.
Quick to prepare, tasty, a pinch of salt and pepper – what’s not to love?
9) Food pairing for snacks
 This is a great tip I picked up from the brilliant Gestational Diabetes UK website – I’m so grateful to them because it solved a riddle for me about snacks. On their website, they say #NeverEatANakedCarb because:
This is a great tip I picked up from the brilliant Gestational Diabetes UK website – I’m so grateful to them because it solved a riddle for me about snacks. On their website, they say #NeverEatANakedCarb because:
Carbs = high blood sugar levels
Carbs + fat + protein = lower blood sugar levels
Food pairing snacks that work for me are:
- Half a green apple with peanut butter dip – so good (any excuse to indulge my peanut butter obsession!)
- Slice of cheddar cheese and half a pear
- Tandoori prawns with mint yoghurt dip
- Houmous, handful of nuts and red pepper
- One slice of peanut butter on toast
- Philadelphia cheese with carrot and celery
- One slice of guacamole on toast
10) There’s taking things too far!
 Early in my new routine, ketones started to show up in my urine at my hospital check ups. Ketones are produced when the body burns fat stores. There can be a number of reasons for this with gestational diabetes – see the Gestational Diabetes UK website for good advice on ketones – but in my case, it was because I restricted carbs too much early on.
Early in my new routine, ketones started to show up in my urine at my hospital check ups. Ketones are produced when the body burns fat stores. There can be a number of reasons for this with gestational diabetes – see the Gestational Diabetes UK website for good advice on ketones – but in my case, it was because I restricted carbs too much early on.
So, the advice from my diabetes team was to add more carbohydrate back into my diet – I enjoyed that check up enormously and the adjustments I made worked.
11) Yes, obviously slabs of cake and ice cream are off the menu in pregnancy, but…
 …occasionally in the last seven weeks, I have given in to my old friend chocolate, paired with a few nuts.
…occasionally in the last seven weeks, I have given in to my old friend chocolate, paired with a few nuts.
Only a couple of squares, mind you! And I let it melt very slowly in the mouth.
After pregnancy, I don’t have to test my blood anymore but I have decided to use my testing kit to learn about the effects of sugary snacks and desserts on my system.
12) Slow down
 Before the GD diagnosis, I wasn’t a fast eater, but I have been learning how to eat my food more mindfully.
Before the GD diagnosis, I wasn’t a fast eater, but I have been learning how to eat my food more mindfully.
I appreciate each mouthful more and savour the food. I experience the textures and tastes more.
Slowing down really helps me to know when I’m full too.
And anyway, the tortoise always beats the hare, right?


 Early the next morning, I phone the diabetes team and ask to be tested as soon as possible. A lovely nurse, Christine, squeezes me in the next morning. They are fully booked, she tells me, but she makes it happen. Christine is ‘minor miracle number one’!
Early the next morning, I phone the diabetes team and ask to be tested as soon as possible. A lovely nurse, Christine, squeezes me in the next morning. They are fully booked, she tells me, but she makes it happen. Christine is ‘minor miracle number one’! 8.30am: I am called through to the nurses’ station for a fasting blood test – as luck would have it, Christine is my nurse. I thank her for such a swift appointment. She has lovely round cheeks when she smiles.
8.30am: I am called through to the nurses’ station for a fasting blood test – as luck would have it, Christine is my nurse. I thank her for such a swift appointment. She has lovely round cheeks when she smiles. Yolanda goes over the information again, slower. I can sense she’s running late for the next appointment but the information does go in better this time. Essentially, if I get two high blood glucose scores, over 5.5 first thing in the morning or over 7.0 after meals, then I should phone the diabetes team and they will discuss medication. She hands me a little book to record my scores. She gives me a prescription to pick up at the hospital pharmacy for metformin – just in case I need it. I already have a monitoring device, which Christine gave to me earlier.
Yolanda goes over the information again, slower. I can sense she’s running late for the next appointment but the information does go in better this time. Essentially, if I get two high blood glucose scores, over 5.5 first thing in the morning or over 7.0 after meals, then I should phone the diabetes team and they will discuss medication. She hands me a little book to record my scores. She gives me a prescription to pick up at the hospital pharmacy for metformin – just in case I need it. I already have a monitoring device, which Christine gave to me earlier.